The Hidden Side of Atrial Fibrillation Medications: Why Ablation is Often the Better Option
- jingxianquah
- Mar 9, 2025
- 3 min read
Updated: Mar 26, 2025
If you’ve been diagnosed with atrial fibrillation (AFib), your doctor may have discussed medications to help control your heart rhythm. While medications can be effective, they’re not always the best long-term solution for everyone. In this post, we’ll summarize the available medications for rhythm control, their potential side effects, and why procedures like ablation are often preferred for maintaining a normal sinus rhythm.
Drugs for Atrial Fibrillation: What You Need to Know
The goal of rhythm control medications is to restore and maintain a normal heart rhythm (sinus rhythm). These medications are often called anti-arrhythmic drugs (AADs). Here’s a breakdown of the most commonly prescribed options:
1. Sodium Channel Blockers
Examples:
Flecainide (Tambocor)
Common Side Effects:
Dizziness or lightheadedness
Nausea
Blurred vision
Rarely, worsening of arrhythmias (pro-arrhythmic effect)
Flecainide is excreted by your liver and kidneys and will require dose adjustments if you have chronic liver/kidney damage.
Flecainide is often used in conjunction with a beta-blocker or calcium channel blocker
2. Potassium Channel Blockers
Examples:
Sotalol (Cardol/Sotalol/Solavert).
Amiodarone (Cordarone/Aratac) - also works through calcium and potassium blocking properties and beta- and alpha-adrenergic receptor blockade
Potential Side Effects:
Fatigue
Prolonged QT interval (A finding on your electrocardiograph, increasing the risk of dangerous arrhythmias)
Bradycardia
Dizziness
Mood changes
Amiodarone specific side effects: - photosensitivity, cataracts, thyroid dysfunction, liver dysfunction, lung fibrosis, neuropathy
Sotalol is excreted by the kidneys and may require dose adjustments if you have chronic kidney disease. Metabolic derangements, such as low potassium levels can potentiate effects of sotalol
Amiodarone toxicity needs to be monitored by your treating physician every six to twelve months with blood tests and CXR.
Why Atrial Fibrillation Medications (AAD) May Not Be the Best Long-Term Solution
While medications can be effective in managing AFib, they’re not without limitations. Here’s why many physicians prefer ablation for long-term rhythm control:
1. Limited Effectiveness
AADs do not cure AFib. Over time, their effectiveness may decrease, and AFib episodes may become more frequent or severe.
Up to 50% of patients on medications will have AF recurrence within the first year, as shown in the AFFIRM trial (below).
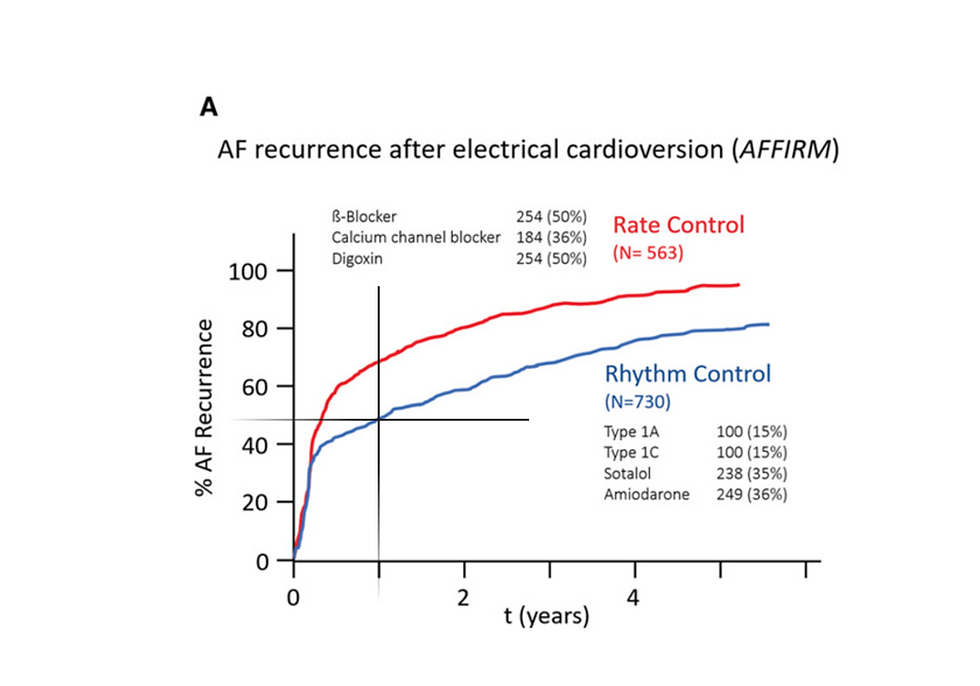
Failure of rhythm control medications (blue line) at one year with AF recurrence approaching 50% of patients in the AFFIRM trial. Ang YS et al. A New Therapeutic Framework for Atrial Fibrillation Drug Development. Circ Res. 2020 Jun 19;127(1):184-201
2. Side Effects
Many anti-arrhythmic drugs have significant side effects, which can impact your quality of life. For example, amiodarone can cause thyroid, lung, or liver problems with long-term use.
Ablation, on the other hand, is a one-time procedure (or occasionally requires a repeat) and doesn’t involve ongoing side effects.
3. Risk of Pro-Arrhythmia
Some medications can actually worsen arrhythmias or cause new ones, a condition known as pro-arrhythmia. This is rare but can be life-threatening.
4. Lifestyle Impact
Medications often require strict adherence to dosing schedules and frequent monitoring (e.g., blood tests for amiodarone or thyroid function).
After a successful ablation, many patients can reduce or even stop their medications, simplifying their treatment plan.
5. Long-Term Outcomes
Ablation has been shown to improve quality of life and reduce the risk of AFib-related complications, such as stroke and heart failure, more effectively than medications.
When Are Medications Still a Good Option?
While ablation is often preferred, medications still play an important role in AFib management, especially for:
Patients who are not candidates for ablation due to other health conditions.
Those who prefer to avoid procedures or are not ready for ablation.
Short-term rhythm control while preparing for ablation or other treatments.
Final Thoughts
Medications can be a helpful tool for managing AFib, but they’re not always the best long-term solution. If you’re struggling with side effects or finding that your medications aren’t controlling your symptoms effectively, talk to your electrophysiologist about whether ablation might be a better option for you.
Disclaimer: This blog post is for informational purposes only and should not replace professional medical advice. Always consult your healthcare provider for personalized guidance.



Comments